How Does Pain Become Chronic: Understanding and Reversing the Cycle
Chronic pain is not just a physical condition; it’s also a learned pattern in the brain. Similar to how we can learn to play the piano or speak a language with practice, our brain can, unfortunately, also learn to produce pain.
How the Brain Learns Pain
Repeated activation of pain signals strengthens neural connections in the brain, making the pain response more efficient over time7. This process, called central sensitization, can cause the nervous system to become overly responsive, leading to heightened sensitivity and long-lasting symptoms.
In one ground-breaking study, researchers looked only at brain scans to predict which patients would recover from back pain and which would develop chronic pain2. Increased connectivity between the nucleus accumbens and the prefrontal cortex was a strong predictor. This suggests that our brain’s response to pain plays a huge role in whether pain fades or lingers3.
The Nervous System’s Response to Pain
When pain strikes, many of us enter a state of nervous system dysregulation. This can show up in four main patterns:
- Fight: frustration, anger, pushing through, over-fixing
- Flight: fear, anxiety, hypervigilance, constant seeking of help
- Fawn: people-pleasing, perfectionism, self-pressure
- Freeze: despair, shutdown, helplessness, emotional numbing
These stress responses can reinforce pain signals, creating a feedback loop that keeps the pain cycle going. We call this feedback loop The Sensitization Cycle.
Fear and the Amplification of Pain
Two studies demonstrate how fear and perception can amplify pain:
- The Scary Picture Study4 showed that people experienced more pain, and even felt pain without a stimulus, when viewing frightening images.
- The Pain-Related Fear Study6 found that individuals with more fear about their pain were more likely to still have pain six months later.
These findings highlight a critical truth: pain is not always a direct reflection of tissue damage, it’s deeply connected to emotional and cognitive factors.
Breaking the Cycle: Evidence-Based Therapies
At Pain Psychotherapy, our goal is to help you shift out of the sensitization cycle and into the desensitization cycle, teaching the brain and body to feel safe again.
We utilize the following two therapy approaches, along with several others, to support clients in entering the desensitization cycle to heal their chronic pain or illness.
Pain Reprocessing Therapy (PRT)
In a landmark clinical trial, 98% of people receiving PRT reported pain reduction, and 66% became pain-free or nearly pain-free, even after an average of 10.7 years of treatment-resistant chronic back pain1. Brain scans showed reduced activity in pain-related brain areas.
Emotional Awareness and Expression Therapy (EAET)
In a study of 230 people with fibromyalgia, EAET significantly reduced widespread pain, with 22.5% of participants experiencing at least a 50% reduction in pain5. By helping clients identify and express emotions safely, EAET calms the nervous system and reduces pain.
Are You Ready to Heal?
Book in for a free 20-minute consultation with one of our therapists to begin your healing journey:
Ashar, Y. K., Gordon, A., Schubiner, H., Uipi, C., Knight, K., Anderson, Z., ... & Wager, T. D. (2021). Effect of pain reprocessing therapy vs placebo and usual care for patients with chronic back pain: A randomized clinical trial. JAMA Psychiatry, 78(11), 1–11.
Baliki, M. N., Petre, B., Torbey, S., Herrmann, K. M., Huang, L., Schnitzer, T. J., ... & Apkarian, A. V. (2012). Corticostriatal functional connectivity predicts transition to chronic back pain. Nature Neuroscience, 15(8), 1117–1119.
Gordon, A., & Ziv, M. (2021). The role of the brain in chronic pain. Pain Medicine, 22(2), 281–289.
Kirwilliam, S. S., & Derbyshire, S. W. G. (2008). Increased bias to report heat or pain following emotional priming with fear. Pain, 137(1), 60–65.
Lumley, M. A., Schubiner, H., Lockhart, N. A., Kidwell, K. M., Harte, S. E., Clauw, D. J., & Williams, D. A. (2017). Emotional awareness and expression therapy, cognitive-behavioral therapy, and education for fibromyalgia: A cluster-randomized controlled trial. Pain, 158(12), 2354–2363.
Picavet, H. S., Vlaeyen, J. W., & Schouten, J. S. (2002). Pain catastrophizing and kinesiophobia: Predictors of chronic low back pain. American Journal of Epidemiology, 156(11), 1028–1034.
Song, Q., Zhang, X., & Liang, Y. (2024). Neural mechanisms of chronic pain sensitization. Neuroscience Bulletin, 40(3), 211–223.
Safe Self-Talk to Support Healing From Chronic Pain and Symptoms
Common negative thoughts about our symptoms can sound like1,2:
- “My symptoms are permanent, and nothing I do helps.”
- “My body is becoming more damaged each day!”
- “Something is really wrong with my body!”
- “My symptoms are only going to worsen over time…”
- “This is hopeless, my body can’t do anything!”
In our approach, we support clients in developing safe self-talk about their symptoms, sensations, emotions, and nervous system state.
Safe self-talk about our symptoms can help the brain reappraise physical sensations and situations as safe, instead of dangerous1,2. However, for safe self-talk to work, our words need to be credible! This is why learning how our nervous system works and relating our pain or symptoms to the criteria for neuroplastic symptoms is so important! To learn more, check out our blog post on Criteria for Neuroplastic Pain.
Examples of Safe Self-Talk for Chronic Symptoms:
- “I know I’m ok; my brain is just misinterpreting normal sensations in my body.”
- “I see how my symptoms are inconsistent, moving around, and triggered by emotions. This shows me it’s neuroplastic, and my body is healthy and capable.”
- “I don’t need to control or change these sensations. There is nothing to fix or figure out!”
- “My body is healthy. My brain is just being overprotective.”
- “It’s physically safe to move this way.”
- “I can respond to my symptoms with deep care and compassion.”
- “I don’t need to like these sensations; I just need to remember they’re safe!”
The goal of using safe self-talk is to reinforce to the brain that it’s safe to feel these symptoms, the body is safe, and movement or activities are safe. Over time, this can support the reduction or elimination of our chronic pain or symptoms 1,2. The key to using brain retraining practices effectively is to do them consistently, but not intensely. You can practice safe self-talk throughout the day, each time you notice a negative thought about your pain or symptoms, and also while engaging in somatic practices with pain or symptoms. As you practice this strategy, please know it’s normal to feel danger and not fully believe our safe self-talk at first! Over time, safe self-talk becomes more natural, effective, and believable.
Now it is your turn to create your own safe self-talk for chronic pain and symptoms. Different phrases work for different people; effective and safe self-talk is unique to you and your symptoms. Find the self-talk that feels right for you! Remember to use the neuroplastic pain or symptom criteria you related to when building your self-talk to make it more credible.
If you need support with your healing, book in for a free 20-minute virtual consultation with one of our therapists:
1. Gordon, A., & Ziv, A. (2021). The way out: A revolutionary, scientifically proven approach to healing chronic pain. Sony/ATV Music Publishing LLC.
2. Pain Reprocessing Therapy Center (2021). Pain reprocessing therapy training.
Medical Trauma: Causes, Signs, and Treatment
By Tanner Murtagh
Medical trauma is a common category of trauma that, unfortunately, often goes unrecognized by physicians or therapists and adequate treatment for it is rarely provided1. It can be defined as a somatic, psychological, or cognitive stress response following a medical procedure1,2.As Levine3 discusses, trauma is not the event that occurred but the response of our nervous system to the event. Trauma is actually prolonged dysregulation in the nervous system, which could look like a fight, flight, freeze, and/or shutdown response3,4.
In my experience working with clients with chronic pain or illness, a large portion of them have medical trauma. Following a surgery, scary procedure, unhelpful treatment, or generally unsupportive or stigmatizing care from medical professionals, many people, for months or years after, have chronic nervous system dysregulation and greatly fear interacting with the medical system.
Causes of medical trauma can include:
- Confusing, scary, or conflicting opinions and information from medical professionals
- Proper education about a procedure not being provided prior to it occurring
- Compassionate support not being provided prior, during, or after a procedure
- Stigma from medical professionals, family, or friends, such as being mistreated or being made to feel “crazy”
- Onset of symptoms due to another health crisis or injury that caused a great sense of danger prior to a procedure
- Experiencing great fear prior to a procedure or surgery occurring
- A sense of inescapable attack was felt before and during a procedure5
- A procedure was unsuccessful or had a bad outcome, resulting in symptoms worsening
- Hope is repeatedly gathered and broken by failed treatments or interventions
Signs of medical trauma can include5,6:
- Prior, during, and/or after a medical procedure a person experiences the following physical symptoms:
- Flight response: anxious, panic, on edge, racing heart, difficulties breathing, tingling, dizziness, racing thoughts, or excessive worry
- Fight response: irritated, angry, racing heart, shortness of breath, high anger towards medical professionals, or rigid movements
- Freeze/shutdown response: shutdown, numb, drowsy, dissociation, floaty sensations, exhaustion, low muscle tone, numbness, poor immune function, or disconnection
- Following the procedure a person has a heightened dysregulated response to routine medical appointments or interactions
- Avoidance of future medical appointments, assessments, or procedures
- Injuries from the procedures, such as scars from a surgery, take longer than normal to heal
- Somatic symptoms, as medical trauma can trigger and perpetuate chronic somatic symptoms such as chronic pain, fatigue, dizziness, and other symptoms
Preventative therapy for medical trauma
Getting psychological treatment prior to an upcoming medical procedure is one of the best ways to prevent medical trauma from occurring5. A well-trained therapist can support somatically processing unpleasant sensations related to upcoming procedures and cognitively processing negative thinking and beliefs regarding it. A therapist can also help in setting up the conditions for a more somatic sense of safety to occur during and after the procedure. This could include5:
- Supporting the individual in educating themselves about the procedure
- Helping the individual in advocating for themselves with the medical team to receive what they need to feel safe
- Aiding an individual in identifying resources of safety they can use during the procedure (e.g. music, supportive person, blanket, or item)
- Supporting an individual in writing a script of instructions for the surgeon or medical team
- Helping an individual gain exposure to being in the hospital while processing sensations
Therapy for Medical Trauma
Once medical trauma has occurred and you have identified it, it can be vital to seek the support of a trained therapist in the area. Our therapists specialize in treating clients with chronic pain or illness and, because of this, are experienced in helping clients in overcoming medical trauma. Collectively, our therapists utilize the following approaches to treat medical trauma:
- Somatic Experiencing
- EMDR
- Somatic Attachment Therapy
- Emotional Awareness & Expression Therapy
- Accelerated Resolution Therapy (ART)
- Radical Exposure Tapping
- Prolonged Exposure Therapy
If you are ready to begin healing from medical trauma or need support to prevent future occurrences, book a free 20-minute consultation with one of our therapists.
McBain, S., & Cordova, M. J. (2024). Medical traumatic stress: Integrating evidence-based clinical applications from health and trauma psychology. Journal of traumatic stress, 37(5), 761–767. https://doi.org/10.1002/jts.23075
Birk, J., Kronish, I., Chang, B., Cornelius, T., Abdalla, M., Schwartz, J., Duer-Hefele, J., Sullivan, A., & Edmondson, D. (2019). The Impact of Cardiac-induced Post-traumatic Stress Disorder Symptoms on Cardiovascular Outcomes: Design and Rationale of the Prospective Observational Reactions to Acute Care and Hospitalizations (ReACH) Study. Health psychology bulletin, 3, 10–20. https://doi.org/10.5334/hpb.16
Levine, Peter A. (1997). Waking the tiger : healing trauma : the innate capacity to transform overwhelming experiences. Berkeley, Calif. :North Atlantic Books,
Dana, D. (2018). The polyvagal theory in therapy: Engaging the rhythm of regulation. W W Norton & Co.
Somatic Experiencing International (2021a). Somatic Experiencing Intermediate year Module 2.
Somatic Experiencing International (2021b). Somatic Experiencing Beginner year Module 1.
What is Pain Reprocessing Therapy?
Can PRT Help in Retraining my Brain out of Chronic Pain and Symptoms?
By Tanner Murtagh, MSW, RSW
For 3 and a half years I experienced widespread chronic pain that continued to worsen over time. To try and reduce or eliminate my chronic pain I did what most people do which included: being examined by several physicians, MRI and x-rays, physiotherapy, chiropractic work, pain medication, and several other physical treatments. However, all the medical tests and treatments did not resolve my pain and in fact, caused my pain to increase.
This is a common story I hear when providing therapy to clients with chronic pain or symptoms. “The medical system has failed me. No treatment is helping.”
The reality is that medical procedures have poor results when it comes to reducing or eliminating chronic pain and symptoms. Surgery, injections, and narcotic pain medications are no more effective than placebo or conservative treatments.1.
So, what is the solution to healing chronic pain and symptoms? The answer lies in the brain. Chronic pain, fatigue, dizziness, or other physical symptoms are often neuroplastic. Neuroplastic pain/symptoms are when the brain changes in such a way that it reinforces chronic pain/symptoms2,3.
When our brain or nervous system feels in emotional danger or dysregulated, chronic pain or symptoms can be triggered and perpetuated2,3. Over time, as pain or symptoms are repeatedly produced, the brain learns to generate these sensations better and better. It is vital to understand that a significant portion of chronic pain and symptoms are neuroplastic, meaning the brain is responsible for triggering and perpetuating them4.
For myself, after 3 and a half years of being in pain I came to understand that my symptoms were neuroplastic in nature. This realization allowed me to shift my focus to rewiring my brain instead of fixing my body. I began to utilize brain retraining exercises, in combination with emotional processing and nervous system regulation, and in doing so over several months I was able to become pain-free.
Research on Pain Reprocessing Therapy (PRT), which is a psychological approach focused on rewiring the brain out of chronic pain, has shown that reversing neuroplastic pain is possible5. In a clinical trial on PRT 66% of participants who received the treatment were able to become pain-free or nearly pain free after 9 sessions5. Over 98% of participants in the study had pain reductions. This research and my personal experience showcase how it is possible to retrain your brain out of chronic pain!
At our clinic we support clients in utilizing brain retraining practices from PRT to heal their chronic pain and symptoms. PRT brain retraining practices for chronic pain and symptoms can include:
Creating New Beliefs about Your Body, Pain, or Symptoms
Understanding that our symptoms are neuroplastic and our body is not permanently damaged is essential. At our clinic, we support people in looking for evidence that their pain or symptoms are in fact neuroplastic. We want to foster the belief that healing is possible. Retraining our brain to develop new beliefs about our body and symptoms, with less fear and more safety, can result in the sensations of pain or symptoms reducing over time 2.
Developing Cognitive Safety Messages
Fearful, frustrated, or despairing thoughts about our pain or symptoms can worsen the sensations2. Brain retraining can involve changing our thoughts about our symptoms by utilizing cognitive safety messages. These could include:
- “I know I’m okay; my brain is just misinterpreting normal sensations in my body.” “I see how my symptoms are inconsistent, moving around, and triggered by emotions. This shows me it’s neuroplastic and my body is healthy and capable.”
- “I don’t need to control or change these sensations. There is nothing to fix or figure out!”
- “My muscles and tendons are healthy. My nerves and ligaments are perfectly intact. My brain is just sensitized and overprotective.”
- “It’s physically safe to move this way.”
- “I don’t need to like the sensations; I just need to remember they’re safe!”
Using messages of safety consistently when you notice yourself having negative thoughts about your symptoms and body can support you in rewiring your brain2. In our clinic, we support people in creating unique messages of safety about their body.
Visualizing Yourself Healing and Moving Your Body
Visualization can be a supportive tool in rewiring the brain. Consistently visualizing yourself becoming pain or symptoms free, being able to approach life again, and being able to exercise and use your body the way you want to can support teaching your brain that your body is healthy and capable.
Somatic Tracking
Often, we have an emotional response of fear, frustration, despair, or annoyance to our pain or symptoms. This negative emotional response to our chronic symptoms can actually worsen our symptoms over time as it increases the level of danger and dysregulation our brain is experiencing2. Somatic tracking is a skill that can support us in changing our emotional response to our chronic pain or symptoms2. Utilizing somatic tracking can teach us to respond to our symptoms with lightness, ease, calmness, and compassion. By changing our emotional response to the symptoms, it can result in our symptoms reducing or becoming eliminated2. Our therapists are experienced in teaching somatic tracking and making it individualized for each client.
Here is a free somatic tracking practice to try:
Graded Exposure to What You Fear
Our natural response to chronic pain or symptoms is to start avoiding anything and everything that could be triggering our symptoms, which can include: certain movements, positions, activities, environments, foods, sounds, or time of day. This causes us to enter into a symptom-avoidance cycle where our symptoms cause us to avoid, the avoidance causes our brain to feel more in danger which triggers more symptoms, more symptoms cause more avoidance, and more avoidance causes more symptoms. We have seen clients stuck in this cycle for decades.
It often isn’t the condition that is triggering our pain or symptoms, but the fact that the brain has learnt to view the condition as dangerous2. Essentially the brain has made a mistaken association between the condition and the symptom. Healing chronic pain and symptoms involves slowly, gently, and compassionately approaching conditions we fear while using somatic tracking to create safety. Approaching these conditions can be REALLY SCARY, however, it supports our brain in breaking these mistaken associations2. This can allow us to live more fully with less pain or symptoms!
Leaning into Pleasant Sensations
When we experience chronic pain or symptoms we get really good at hyper-focusing on unpleasant sensations in our body. Part of retraining our brain is teaching it to focus on pleasant sensations. Consistent practice of leaning into pleasant sensations cultivates nervous system regulation and supports the brain in more easily gravitating towards these sensations in the future2. Leaning into pleasant sensations could look like:
- Feeling the warmth of the sun on your skin
- Feeling the pleasant sensations of breathing slowly
- Noticing loose or relaxed sensations in your body
- Attending to sights or sounds that are calming
- Enjoying a warm coffee or tea
- Using soothing touch (making circles on your chest or giving yourself a hug)
Conclusion
As you can see there are many ways we can utilize PRT to retrain our brain out of chronic pain or symptoms. If physical treatments have provided limited results in healing your symptoms, it may be time to start focusing on treating the brain.
If you need support with your healing book in for a free 20-minute consultation with one of our therapists.
Deyo, R. A., Mirza, S. K., Turner, J. A., & Martin, B. I. (2009). Overtreating chronic back pain: time to back off?. Journal of the American Board of Family Medicine : JABFM, 22(1), 62–68. https://doi.org/10.3122/jabfm.2009.01.080102
Pain Reprocessing Therapy Center (2021). Pain reprocessing therapy training.
Gordon, A., & Ziv, A. (2021). The way out: A revolutionary, scientifically proven approach to healing chronic pain. Sony/ATV Music Publishing LLC.
Woolf C. J. (2011). Central sensitization: implications for the diagnosis and treatment of pain. Pain, 152(3 Suppl), S2–S15. https://doi.org/10.1016/j.pain.2010.09.030
Ashar, Y. K., Gordon, A., Schubiner, H., Uipi, C., Knight, K., Anderson, Z., Carlisle, J., Polisky, L., Geuter, S., Flood, T. F., Kragel, P. A., Dimidjian, S., Lumley, M. A., & Wager, T. D. (2022). Effect of Pain Reprocessing Therapy vs Placebo and Usual Care for Patients With Chronic Back Pain: A Randomized Clinical Trial. JAMA psychiatry, 79(1), 13–23. https://doi.org/10.1001/jamapsychiatry.2021.2669
What Symptoms or Conditions Can Be Neuroplastic?
By Tanner Murtagh, MSW, RSW
Neuroplastic pain and symptoms are caused and amplified by the brain and nervous system processes and are not due to disease or structural damage in the body. Put simply, pain or symptoms are felt even though the body is structurally healthy or has healed from an injury. The brain continues to generate pain or symptoms due to negative thoughts or beliefs, emotions, and a dysregulated nervous system1,2.
The brain is responsible for generating pain and symptom sensations. When the brain receives signals from the body, it combines that information with a large amount of data already present in the brain. This means our emotions, nervous system state, memories, and beliefs about the health of our body greatly influence if, or how much, pain or symptoms are generated3.
One of the most common questions we are asked is, “What types of symptoms can be neuroplastic?” It is vital to understand a significant portion of chronic pain and symptoms are neuroplastic in nature4.
Here is a list of conditions that can be fully neuroplastic or have a neuroplastic component1:
- Fibromyalgia
- Chronic neck and back pain
- Abdominal and pelvic pain
- Irritable bowel syndrome
- Non-ulcer dyspepsia
- Headaches & migraines
- Complex regional pain syndrome (CRPS)
- Vestibular concerns and dizziness
- Tinnitus
- Chronic fatigue syndrome (CFS)
- Postural orthostatic tachycardia syndrome (POTS)
- Myofascial pain syndrome
- Chemical sensitivities
- Irritable bladder syndrome (interstitial cystitis)
Our therapists specialize in treating neuroplastic pain and symptoms. If you are ready to begin your healing journey, book in for a free 20-minute consultation with one of our therapists.
Clarke, D. D., & Schubiner, H. (2019). Introduction. In D. Clarke, H. Schubiner, M. Clarke-Smith, & A. Abbass (Eds.), Psychophysiologic disorders: Trauma informed, interprofessioal diagnosis and treatment (pp. 5-25). Psychophysiologic Disorders Association.
Gordon, A., & Ziv, A. (2021). The way out: A revolutionary, scientifically proven approach to healing chronic pain. Sony/ATV Music Publishing LLC.
Pain Reprocessing Therapy Center (2021). Pain reprocessing therapy training.
Woolf C. J. (2011). Central sensitization: implications for the diagnosis and treatment of pain. Pain, 152(3 Suppl), S2–S15. https://doi.org/10.1016/j.pain.2010.09.030
What is Dysregulating Your Nervous System?
Information you need to know to Heal Your Chronic Pain and Symptoms
By Tanner Murtagh, MSW, RSW
Chronic dysregulation of the nervous system is when you get stuck in the states fight, flight, freeze, or shutdown for prolonged periods of time1. When prolonged dysregulation occurs, your nervous system can then become sensitized, meaning it begins to generate chronic pain and/or symptoms.
A healthy nervous system is a flexible system that shifts with ease between different states1. This doesn’t mean you will always feel calm or relaxed, but instead, you are able to flexibly shift with ease out of states of fight, flight, freeze, or shutdown. Our therapeutic approach with clients supports them in becoming more regulated and flexible, and in our experience, this can support the reduction or complete dissipation of chronic pain and symptoms.
An essential step in regulating the nervous system is first understanding the factors that are causing you to become dysregulated. These factors could include but are not limited to:
- Trauma1, 2
- Childhood adversity3
- Chronic stress3
- Burnout4
- Social isolation5
- Perfectionism6
- Suppressing difficult emotions7
- Poor sleep8
- Lack of exercise9
- Poor diet10
- Premature birth11, 12
- Dangerous and oppressive social factors13, 14, 15
It is important to reflect on if you relate to any of these factors as understanding what factors are dysregulating you can support you in knowing where you need to focus your healing work. Remember this can support you in eliminating your chronic pain or symptoms.
Our therapists are trained in assessing a client in what factors are dysregulating them early on in treatment and a unique treatment plan is then developed based on this.
If you are ready to begin regulating your nervous system and reduce your chronic pain and symptoms, book in for a free 20-minute consultation with one of our therapists.
1. Dana, D. (2018). The polyvagal theory in therapy: Engaging the rhythm of regulation. W W Norton & Co.
2. Schneider, M., & Schwerdtfeger, A. (2020). Autonomic dysfunction in posttraumatic stress disorder indexed by heart rate variability: a meta-analysis. Psychological medicine, 50(12), 1937–1948. https://doi.org/10.1017/S003329172000207X
3. Elbers, J., Jaradeh, S., Yeh, A. M., & Golianu, B. (2018). Wired for Threat: Clinical Features of Nervous System Dysregulation in 80 Children. Pediatric neurology, 89, 39–48. https://doi.org/10.1016/j.pediatrneurol.2018.07.007
4. Kanthak, M. K., Stalder, T., Hill, L. K., Thayer, J. F., Penz, M., & Kirschbaum, C. (2017). Autonomic dysregulation in burnout and depression: evidence for the central role of exhaustion. Scandinavian journal of work, environment & health, 43(5), 475–484. https://doi.org/10.5271/sjweh.3647
5. Grippo, A. J., Lamb, D. G., Carter, C. S., & Porges, S. W. (2007). Social isolation disrupts autonomic regulation of the heart and influences negative affective behaviors. Biological psychiatry, 62(10), 1162–1170. https://doi.org/10.1016/j.biopsych.2007.04.011
6. Afshar, H., Roohafza, H., Sadeghi, M., Saadaty, A., Salehi, M., Motamedi, M., Matinpour, M., Isfahani, H. N., & Asadollahi, G. (2011). Positive and negative perfectionism and their relationship with anxiety and depression in Iranian school students. Journal of research in medical sciences : the official journal of Isfahan University of Medical Sciences, 16(1), 79–86.
7. Patel, Jainish & Patel, Prittesh. (2019). Consequences of Repression of Emotion: Physical Health, Mental Health and General Well Being. International Journal of Psychotherapy Practice and Research. 1. 16-21. 10.14302/issn.2574-612X.ijpr-18-2564.
8. Hirotsu, C., Tufik, S., & Andersen, M. L. (2015). Interactions between sleep, stress, and metabolism: From physiological to pathological conditions. Sleep science (Sao Paulo, Brazil), 8(3), 143–152. https://doi.org/10.1016/j.slsci.2015.09.002
9. Schuch, F. B., & Vancampfort, D. (2021). Physical activity, exercise, and mental disorders: it is time to move on. Trends in psychiatry and psychotherapy, 43(3), 177–184. https://doi.org/10.47626/2237-6089-2021-0237
10. Kris-Etherton, P. M., Petersen, K. S., Hibbeln, J. R., Hurley, D., Kolick, V., Peoples, S., Rodriguez, N., & Woodward-Lopez, G. (2021). Nutrition and behavioral health disorders: depression and anxiety. Nutrition reviews, 79(3), 247–260. https://doi.org/10.1093/nutrit/nuaa025
11. Mulkey, S. B., & du Plessis, A. J. (2019). Autonomic nervous system development and its impact on neuropsychiatric outcome. Pediatric research, 85(2), 120–126. https://doi.org/10.1038/s41390-018-0155-0
12. Pyhälä, R., Wolford, E., Kautiainen, H., Andersson, S., Bartmann, P., Baumann, N., Brubakk, A. M., Evensen, K. A. I., Hovi, P., Kajantie, E., Lahti, M., Van Lieshout, R. J., Saigal, S., Schmidt, L. A., Indredavik, M. S., Wolke, D., & Räikkönen, K. (2017). Self-Reported Mental Health Problems Among Adults Born Preterm: A Meta-analysis. Pediatrics, 139(4), e20162690. https://doi.org/10.1542/peds.2016-2690
13. Goosby, B. J., Cheadle, J. E., & Mitchell, C. (2018). Stress-Related Biosocial Mechanisms of Discrimination and African American Health Inequities. Annual review of sociology, 44(1), 319–340. https://doi.org/10.1146/annurev-soc-060116-053403
14. Brandt, L., Liu, S., Heim, C., & Heinz, A. (2022). The effects of social isolation stress and discrimination on mental health. Translational psychiatry, 12(1), 398. https://doi.org/10.1038/s41398-022-02178-4
15. Caldwell, J. A., Borsa, A., Rogers, B. A., Roemerman, R., & Wright, E. R. (2023). Outness, Discrimination, and Psychological Distress Among LGBTQ+ People Living in the Southern United States. LGBT health, 10(3), 237–244. https://doi.org/10.1089/lgbt.2021.0295
Are you Traumatized from your Chronic Pain and Symptoms?
In this blog post we discuss what trauma actually is, the link between trauma and chronic pain/symptoms, and how we can experience chronic pain/symptoms as traumatic.
Defining Trauma
Trauma is not the event that occurred, but our autonomic nervous system response1. The same event could be traumatizing for one person, and not for another. It’s not black and white; trauma can be more and less severe in its impact. Trauma can be defined as nervous system dysregulation, including an overactive sympathetic and/or dorsal vagal state, that remains stuck in the body1.
Symptoms of trauma can look like:
Overactivation of the sympathetic system:
- Physical symptoms: difficulty breathing, increased heart rate, difficulties or inability to sleep, tingling, cold sweats, dizziness, chronic pain, tension, tinnitus and other physical symptoms1,2
- Mental symptoms: racing thoughts, worry and obsessive thinking, anxiety, irritation, panic, or rage1,2
Overactivation of the dorsal vagal system:
- Physical symptoms: exhaustion, low energy, low muscle tone, numbness, poor immune function, issues with digestion, chronic pain/symptoms, and chronic fatigue1,2
- Mental symptoms: lacking motivation or interest, dissociation, depression, numb, disconnection in relationships, lack of responsiveness1,2
So why does this matter when it comes to chronic pain and symptoms? It matters because when we experience trauma, our nervous system can become sensitized meaning chronic pain, fatigue, dizziness, and/or other chronic symptoms are triggered.
Trauma and Chronic Pain/Symptoms
There are major links between trauma and chronic symptoms:
- Adults are 2.7 times more likely to have chronic widespread pain if they have significant trauma in their past3
- A meta-analysis study on trauma showed a significantly increased likelihood of developing Fibromyalgia and a 4-time higher likelihood of developing chronic fatigue syndrome4
- Chronic nervous system dysregulation is associated with inflammatory bowel diseases, functional digestive disorders, and IBS5,6
- PTSD is associated with higher rates of dizziness/vestibular concerns7
These studies teach us that trauma can be a factor in triggering and perpetuating chronic pain and symptoms. Our nervous system lets us know, through chronic pain and symptoms, that it is feeling dysregulated and in a state of survival. As Deb Dana states, “Trauma replaces patterns of connection with patterns of protection”8, and because of this shift, we become much more likely to develop chronic symptoms. This is why trauma is a major factor that we focus on when treating chronic pain and symptoms.
Now let’s discuss one specialized type of trauma that commonly occurs when we are experiencing chronic pain and symptoms, which we call sensitization trauma.
Sensitization Trauma
When we experience chronic pain or symptoms, we can experience what we refer to as sensitization trauma. Sensitization trauma is trauma that occurs during the onset, progression, or relapse of chronic pain/symptoms, resulting in our nervous system having an overactive sympathetic (fight/flight) and/or dorsal vagal (freeze/shutdown) response. Unfortunately, sensitization trauma being untreated can result in chronic pain and symptoms worsening over time.
Sensitization trauma occurs because:
- We feel dysregulated by the onset, progression, or relapse of symptoms
- Fear, confusion, frustration, or hopelessness while trying to diagnose the problem and dealing with the medical system
- Stigma from medical practitioners or individuals in our lives (being mistreated or being made to feel “crazy”)
- The onset of symptoms occurring due to another health crisis or injury that caused a sense of high danger
- Scary physical procedures or surgeries
- Made worse if treatments weren’t helpful
- Significant reduction in ability and change in lifestyle
- Hope is gathered and broken by failed treatments or interventions
Releasing Sensitization Trauma
For many people with chronic pain and symptoms, sensitization trauma needs to be processed for symptoms to reduce or dissipate. At our clinic, we provide a somatic approach to clients to support them in healing their sensitization trauma. This can result in our chronic pain or symptoms reducing or dissipating.
If you are ready to begin your healing journey from trauma and chronic symptoms, reach out to one of our therapists to book a free 20-minute consultation.
Somatic Experiencing International (2021). Somatic Experiencing Beginner year Module 1.
Anda, R. F., Felitti, V. J., Bremner, J. D., Walker, J. D., Whitfield, C., Perry, B. D., Dube, S. R., & Giles, W. H. (2006). The enduring effects of abuse and related adverse experiences in childhood: A convergence of evidence from neurobiology and epidemiology. European Archives of Psychiatry and Clinical Neuroscience 256, 174-186.
Afari, N., Ahumada, S. M., Wright, L. J., Mostoufi, S., Golnari, G., Reis, V., & Cuneo, J. G. (2014). Psychological trauma and functional somatic syndromes: a systematic review and meta-analysis. Psychosomatic medicine, 76(1), 2–11. https://doi.org/10.1097/PSY.0000000000000010
Bonaz, B., Sinniger, V., & Pellissier, S. (2016). Vagal tone: effects on sensitivity, motility, and inflammation. Neurogastroenterology and motility : the official journal of the European Gastrointestinal Motility Society, 28(4), 455–462. https://doi.org/10.1111/nmo.12817
Pellissier, S., Dantzer, C., Mondillon, L., Trocme, C., Gauchez, A. S., Ducros, V., Mathieu, N., Toussaint, B., Fournier, A., Canini, F., & Bonaz, B. (2014). Relationship between vagal tone, cortisol, TNF-alpha, epinephrine and negative affects in Crohn's disease and irritable bowel syndrome. PloS one, 9(9), e105328. https://doi.org/10.1371/journal.pone.0105328
Haber, Y. O., Chandler, H. K., & Serrador, J. M. (2016). Symptoms Associated with Vestibular Impairment in Veterans with Posttraumatic Stress Disorder. PloS one, 11(12), e0168803. https://doi.org/10.1371/journal.pone.0168803
Dana, D. (2019). 2-Day Workshop: Polyvagal Theory Informed Trauma Assessment and Interventions
Polyvagal Theory and Chronic Pain and Symptoms
By Tanner Murtagh, MSW, RSW
At our clinic, we utilize Polyvagal Theory to support clients in reducing their chronic pain or symptoms. In this post we’ll explore Polyvagal Theory, providing education on the nervous system, and how this relates to your neuroplastic pain and symptoms.
Our human bodies contain a built-in hierarchy of responses, meaning we shift between three systems depending on safety or danger. Our nervous system detects and interprets signals of either safety or danger and guides what system we shift into1.
The Parasympathetic Branch
Your parasympathetic branch consists of your vagus nerve, the 10th cranial nerve and the longest of the cranial nerves1, 2.
The vagus nerve facilitates bidirectional communication between the body and brain:
- 80% of safety or danger signals are sensory, meaning they come from the body and go to the brain.
- Only 20% of safety or danger signals are motor, meaning the messages come directly from the brain1, 2.
This is why safety starts in the body! While thinking and beliefs are important, we are greatly influenced by our nervous system state. To fully heal trauma, mental health problems, and chronic pain/symptoms, we need to regulate the nervous system. At our clinic we focus our treatment on this.
The vagus nerve travels from the brainstem at the base of the skull in 2 directions1, 2:
- Downward through the lungs, heart, diaphragm, and stomach.
- Upward to connect with nerves in the neck, throat, eyes, and ears.
The vagus nerve is split into two parts: the ventral vagal system and the dorsal vagal system.
The Dorsal Vagal System
Evolutionarily, this system is 500 million years old! The dorsal vagal system is unmyelinated, comes down the back of the body, and is located below the diaphragm1, 2.
The dorsal vagal system responds to signals of extreme danger, causing us to freeze, disconnect, dissociate, feel numb or depressed, and protect ourselves by going into a state of shutdown and collapse1, 2.
The Ventral Vagal System
Evolutionarily, this system is 200 million years old! The ventral vagal system is myelinated, comes down the front of the body, and is located above the diaphragm1, 2.
The ventral vagal system responds to signals of safety, allowing us to feel socially connected, engaged, and safe. Part of the ventral vagal system is the social engagement system which controls facial expression, social gaze, middle ear muscles, ingestion, vocalizing, swallowing, breathing, orienting, and social gesturing1, 2.
The Sympathetic Branch
Evolutionarily, the sympathetic system is 400 million years old! It is found in the midsection of the spinal cord1, 2.
The sympathetic system mobilizes us for action, responding to signals of danger by triggering our fight or flight response. But, it’s more than just fight or flight! It provides energy to live – excitement, play or passion1, 2.
Shifting Within the Autonomic Nervous System
The autonomic nervous system shifts between ventral vagal, sympathetic, and dorsal vagal based on neuroception1, 2.
- Signals of safety → ventral vagal activation (connected, safe, social, calm) 1, 2
- Signals of danger → sympathetic system activation (mobilize to fight or flee) 1, 2
- Often, taking action helps us restore safety and shift back to the ventral vagal system
- High, inescapable, and persistent danger → dorsal vagal activation (freeze, shut down, and collapse to survive) 1, 2
- This may also be a helpful survival option!
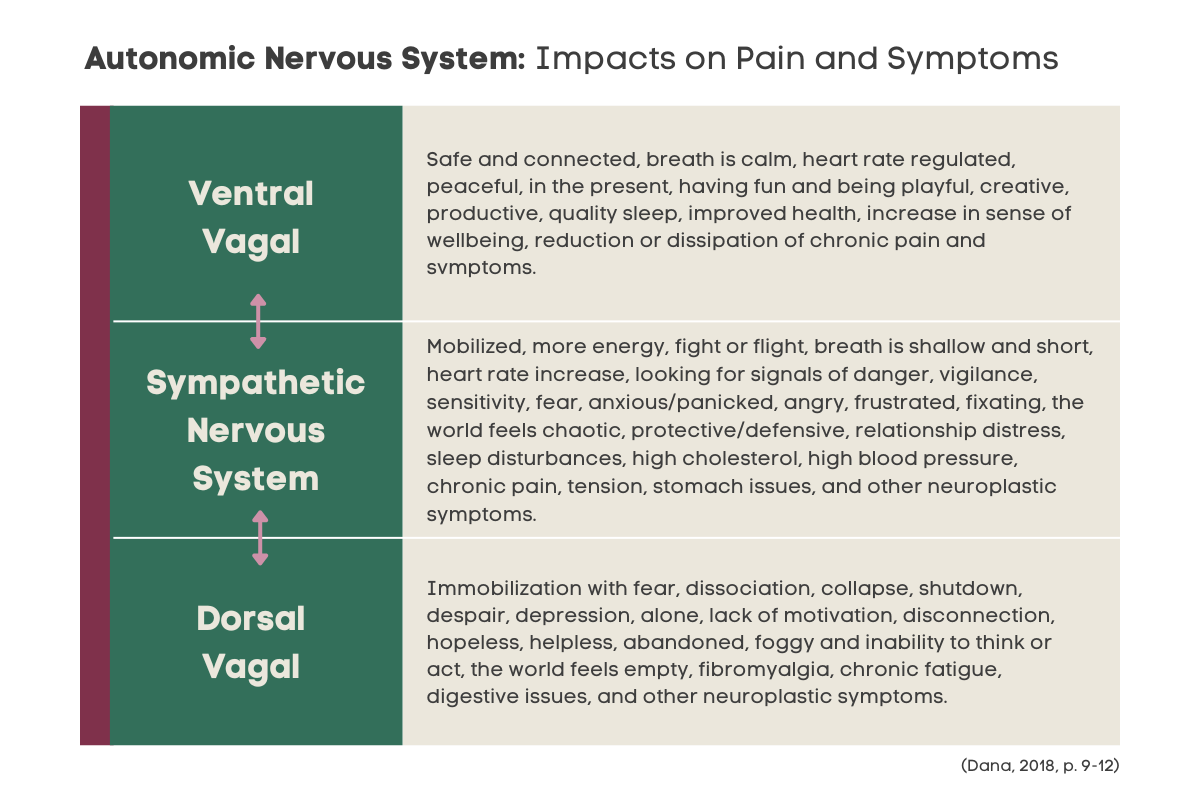
This chart shows how we typically experience the three different systems and how they can impact pain and symptoms:
An important note: Briefly shifting into the sympathetic or dorsal vagal systems is healthy as long as we’re able to shift back to safety with ease. It’s when we’re dysregulated for prolonged periods of time that our nervous system becomes sensitized, triggering and perpetuating chronic pain and symptoms 1, 2.
A key focus for our therapists when collaborating with clients is to assist their nervous system in accurately recognizing signals of safety and danger, both internally and externally. This allows the nervous system the ability to shift more easily to a ventral vagal state after they experience stressors. We support clients in learning how to connect with their body and understand what state they are in. This is a vital step in having a client’s chronic pain and symptoms reduced.
To begin your healing, book a free 20-minute consultation with one of our therapists:
Dana, D. (2018). The polyvagal theory in therapy: Engaging the rhythm of regulation. W W Norton & Co.
Porges, S. W. (2019) Clinical Applications of the Polyvagal Theory.
Dana, D. (2019). 2-Day Workshop: Polyvagal Theory Informed Trauma Assessment and Interventions