Treatment
AT PAIN PSYCHOTHERAPY CANADA WE SPECIALIZE IN TREATING CHRONIC PAIN AND SYMPTOMS
Studies have shown that chronic pain and symptoms such as back pain, fibromyalgia, pelvic pain, neck pain, migraines, headaches, IBS, fatigue, dizziness, and tinnitus are often not structurally caused, but occur in the brain due to learned neural pathways1,2. At Pain Psychotherapy Canada, we specialize in treatment approaches that help our clients heal these brain and nervous system issues.
For example, a recent study completed in Boulder, Colorado found the majority of participants with chronic back pain, who received Pain Reprocessing Therapy, were pain free or nearly pain free one year later2. Furthermore, somatic (body-focused) therapies are shown to reduce pain symptoms3.
Over the years, non-structural chronic pain and symptoms have gone by many names, including Tension Myoneural Syndrome (TMS), Mind-Body Syndrome, Psychophysiologic Disorder, Psychosomatic Pain, Somatic Pain, Somatoform Disorder, Somatic Symptom Disorder, Nociplastic Pain and Neuroplastic Pain. While people diagnosed with these conditions may feel invalidated, studies show us pain with no structural/physical cause is real and occurs in the brain1,4.
“Pain is a danger signal”5,6. It’s job is to protect you. However, our pain systems can become over-protective, activating pain in the absence of structural problems, or persisting after an injury has healed. The brain misinterprets safe signals from the body as painful due to learned beliefs about the body, emotions, and the state of our nervous system6. When this miscommunication occurs, it is known as neuroplastic pain or mind-body concerns. With appropriate treatment it can be reversed.
A helpful analogy is to think about neuroplastic pain like an over-protective guard dog. A knock at the door may be a friendly visitor, but the reactive dog becomes too alarmed and starts barking. Research shows us that when the brain receives signals from the body, “cognitive and emotional factors have a critically important influence on pain perception”7, meaning an over-protective brain can generate too much pain. Our job is to help you retrain the pain system in your brain, so it becomes less reactive and pain-generating.
A question that we commonly hear is: Why does our brain react this way to safe physical sensations?
Safe sensations are amplified into pain when our brain and nervous system feels in danger5. The following factors can trigger and perpetuate neuroplastic pain and mind-body symptoms6,8:
- Belief the body is permanently damaged or flawed
- Responding to our pain or symptoms with fear, worry, frustration, despair, grief, or anger
- Anxious and depressive symptoms
- Unprocessed trauma impacting nervous system functioning
- Nervous system dysregulation, meaning being stuck in a fight, flight, freeze, or shutdown state for prolonged periods of time
- High-alert behaviours such as perfectionism, people-pleasing, placing pressure on ourselves, excessive control, self-criticism, worrying, and/or obsessive thinking
- Social and environmental factors that create a sense of danger
To help our clients reduce or eliminate pain, our treatment model focusing on increasing the sense of safety in the brain and nervous system. This involves changing unhelpful beliefs, increasing your sense of safety with physical sensations and emotions, regulating your nervous system, processing trauma, improving social and environmental safety, and gradually getting back to activities.
Our Treatment Approach
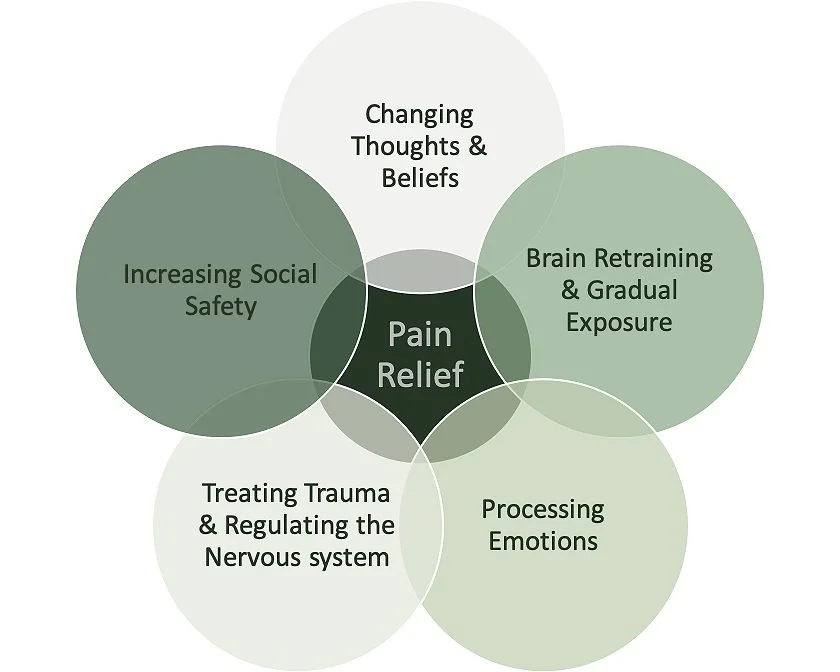
Our approach utilizes tools and education from Pain Reprocessing Therapy, Polyvagal Theory, Emotional Awareness and Expression Therapy, and other cognitive, somatic, behavioural, and trauma-focused therapies, to treat chronic pain and symptoms. We use a detailed and holistic approach focused on 5 main areas:
CHANGING THOUGHTS AND BELIEFS Gathering evidence for physical safety:
Most often, our work begins with an assessment for neuroplastic pain. We engage in a detailed assessment, where we look for evidence that a client’s pain is not behaving in ways consistent with a structural injury or disease. Gathering evidence your pain is neuroplastic is a very important step toward changing your beliefs about your pain, increasing safety in your body, and shifting your reaction to sensations2,6.
Developing safer thinking patterns and beliefs
Chronic pain invites the mind to think negatively. Many of our clients experience fixation on their symptoms, negative views about their bodies, worry about the future, fear of activities that may cause pain, self-judgment, and spend a lot of time trying to diagnose or find a cure. We help our clients shift toward more helpful, hopeful, compassionate, and empowered thinking habits that increase their safety and reduce pain.
RETRAINING THE BRAIN THROUGH GRADUAL EXPOSURE Practicing safer responses to physical sensations
Strategies from Pain Reprocessing Therapy help “retrain the brain to respond to sensations from the body properly, and subsequently break the cycle of chronic pain”6. Somatic tracking is one of the primary techniques utilized in Pain Reprocessing Therapy, which can be understood as a form of exposure that utilizes three aspects: mindfulness, safety reappraisal, and positive affect induction5,6. The aim of somatic tracking is to help clients facilitate corrective experiences, where they feel safe with sensations occurring in their body. This heals the communication between mind and body, reducing pain over time.
Understanding conditioned responses
Research on brain activity shows us how, unlike new or acute injuries, chronic pain involves the activation of our memory systems9. Pain is a protector, and our brains make associations between pain and the activity/condition that was happening when it flared up6. This means the next time you engage in a similar activity or condition (examples can include movements, foods, weather, noises, crowded places, etc.) our brain may become over-protective and generate more pain. By gathering evidence of physical safety and education on how the pain system works, our clients often realize their brain is being over-protective in many conditions that are physically safe.
Reducing fear-based avoidance
The principles of exposure therapy are important in our approach. As our clients gain confidence in their safety, we help them reduce avoidance behaviours and gently expand their movement and activity. Through gradual exposure, our brains gain new evidence for safety by witnessing us engaging in tasks that used to feel dangerous or impossible6. When the brain realizes it no longer needs to protect us, fear and pain sensations go extinct6. This allows our clients to engage more fully in life again.
PROCEESSING EMOTIONS Learning to feel safe with emotions
Studies have found that similar areas of the brain are activated during both emotional pain and physical pain, and resisting or supressing difficult emotions can increase pain sensations10,11. We help our clients learn to fully feel and allow difficult emotions their body, cultivating a sense of safety. By increasing our safety with our emotions, pain and symptoms reduce12.
Developing strategies that allow emotions to help and guide us
At our clinic we utilize somatic therapies and Emotional Awareness and Expression Therapy to support clients in better approaching, understanding, and allowing emotions in their body12. Our goal is to help our clients in becoming fully embodied beings, where the emotions and sensations they feel in their bodies become helpful signals that can guide them toward self-expression and their values.
TREATING TRAUMA AND REGULATING THE NERVOUS SYSTEM Developing polyvagal skills to regulate the nervous system
When our nervous system becomes chronically dysregulated and stuck in a fight, flight, freeze, or shutdown state, we become prone to developing chronic pain, chronic fatigue, and IBS13,14,15,16. Factors that can contribute to nervous system dysregulation include trauma17,18, Childhood adversity19, Chronic stress19, Burnout20, Social Isolation21, Perfectionism22, Suppressing difficult emotions23, Poor sleep24, and premature birth25,26. Our therapists use a Polyvagal-informed approach to support clients in developing a better relationship with their nervous system and gain skills to regulate it.
Processing trauma
To facilitate nervous system regulation, we help our clients process trauma, utilizing somatic experiencing, somatic attachment, Accelerated Resolution Therapy (ART), EMDR, Radical Exposure Tapping, and Prolonged Exposure Therapy. These approaches help our clients process memories and reduce the cognitive and emotional impacts of past events, leading to reduced nervous system reactivity and greater safety. A safer and more regulated nervous system experiences less chronic pain and symptoms.
INCREASING SOCIAL SAFETY Improving Relationships
Experiencing concerns with attachment, conflict, loneliness, boundaries and abuse can create a sense of danger in our mind and body, causing and amplify pain27. We utilize systemic approaches to help our clients increase safety and improve relationships with family, intimate partners, friends, and workplaces.
Addressing the impacts of systemic oppression
Chronic stress from oppression of our body, sexuality, gender, racial identity, cultural differences, and/or neurodiversity can cause and amplify pain28,29. We utilize affirming and anti-oppressive counselling approaches to help our clients develop a sense of safety within their bodies and identities, navigate oppression, and increase their social safety to improve mental health and reduce pain.
To begin your journey out of chronic pain, contact us today and schedule a free 20-minute consultation with one of our therapists!
Woolf C. J. (2011). Central sensitization: implications for the diagnosis and treatment of pain. Pain, 152(3 Suppl), S2–S15. https://doi.org/10.1016/j.pain.2010.09.030
Ashar, Y. K., Gordon, A., Schubiner, H., Uipi, C., Knight, K., Anderson, Z., Carlisle, J., Polisky, L., Geuter, S., Flood, T. F., Kragel, P. A., Dimidjian, S., Lumley, M. A., & Wager, T. D. (2022). Effect of Pain Reprocessing Therapy vs Placebo and Usual Care for Patients With Chronic Back Pain: A Randomized Clinical Trial. JAMA psychiatry, 79(1), 13–23. https://doi.org/10.1001/jamapsychiatry.2021.2669
Andersen, T.E., Ellegaard, H., Schiøttz-Christensen, B. et al. Somatic experiencing® for patients with low back pain and comorbid posttraumatic stress disorder – protocol of a randomized controlled trial. BMC Complement Altern Med 18, 308 (2018). https://doi.org/10.1186/s12906-018-2370-y
Derbyshire, S. W., Whalley, M. G., Stenger, V. A., Oakley, D. A. (2004) Cerebral activation during hypnotically induced and imagined pain. Neuroimage, 23(1), 392-401.
Gordon, A., Ziv, A. (2021). The way out: A revolutionary, scientifically proven approach to healing chronic pain. Sony/ATV Music Publishing LLC.
Pain Reprocessing Therapy Center (2021). Pain reprocessing therapy training.
Crofford LJ. Chronic Pain: Where the Body Meets the Brain. Trans Am Clin Climatol Assoc. 2015;126:167-83. PMID: 26330672; PMCID: PMC4530716.
Dana, D. (2018). The polyvagal theory in therapy: Engaging the rhythm of regulation. WW Norton & Co.
Hashmi, J. A., Baliki, M. N., Huang, L., Baria, A. T., Torbey, S., Hermann, K. M., Schnitzer, T. J., & Apkarian, A. V. (2013). Shape shifting pain: chronification of back pain shifts brain representation from nociceptive to emotional circuits. Brain : a journal of neurology, 136(Pt 9), 2751–2768. https://doi.org/10.1093/brain/awt211
Burns, J. W., Quartana, P. J., & Bruehl, S. (2008). Anger inhibition and pain: Conceptualizations, evidence and new directions. Journal of Behavioral Medicine, 31, 259 –279. http://dx.doi.org/10.1007/s10865-008- 9154-7
Kross, E., Berman, M. G., Mischel, W., Smith, E. E., Wager, T. D. (2011). Social rejection shares somatosensory representations with physical pain. Proceedings of the National Academy of Sciences of the USA, 108, 6270-6275.
Lumley, M. A., Schubiner, H., Lockhart, N. A., Kidwell, K. M., Harte, S. E., Clauw, D. J., & Williams, D. A. (2017). Emotional awareness and expression therapy, cognitive behavioral therapy, and education for fibromyalgia: a cluster-randomized controlled trial. Pain, 158(12), 2354–2363. https://doi.org/10.1097/j.pain.0000000000001036
Bonaz, B., Sinniger, V., & Pellissier, S. (2016). Vagal tone: effects on sensitivity, motility, and inflammation. Neurogastroenterology and motility : the official journal of the European Gastrointestinal Motility Society, 28(4), 455–462. https://doi.org/10.1111/nmo.12817
Pellissier, S., Dantzer, C., Mondillon, L., Trocme, C., Gauchez, A. S., Ducros, V., Mathieu, N., Toussaint, B., Fournier, A., Canini, F., & Bonaz, B. (2014). Relationship between vagal tone, cortisol, TNF-alpha, epinephrine and negative affects in Crohn's disease and irritable bowel syndrome. PloS one, 9(9), e105328. https://doi.org/10.1371/journal.pone.0105328
Koenig, J., Loerbroks, A., Jarczok, M. N., Fischer, J. E., & Thayer, J. F. (2016). Chronic Pain and Heart Rate Variability in a Cross-Sectional Occupational Sample: Evidence for Impaired Vagal Control. The Clinical journal of pain, 32(3), 218–225. https://doi.org/10.1097/AJP.0000000000000242
Van Cauwenbergh, D., Nijs, J., Kos, D., Van Weijnen, L., Struyf, F., & Meeus, M. (2014). Malfunctioning of the autonomic nervous system in patients with chronic fatigue syndrome: a systematic literature review. European journal of clinical investigation, 44(5), 516–526. https://doi.org/10.1111/eci.12256
Schneider, M., & Schwerdtfeger, A. (2020). Autonomic dysfunction in posttraumatic stress disorder indexed by heart rate variability: a meta-analysis. Psychological medicine, 50(12), 1937–1948. https://doi.org/10.1017/S003329172000207X
Dana, D. (2019). 2-Day Workshop: Polyvagal Theory Informed Trauma Assessment and Interventions
Elbers, J., Jaradeh, S., Yeh, A. M., & Golianu, B. (2018). Wired for Threat: Clinical Features of Nervous System Dysregulation in 80 Children. Pediatric neurology, 89, 39–48. https://doi.org/10.1016/j.pediatrneurol.2018.07.007
Kanthak, M. K., Stalder, T., Hill, L. K., Thayer, J. F., Penz, M., & Kirschbaum, C. (2017). Autonomic dysregulation in burnout and depression: evidence for the central role of exhaustion. Scandinavian journal of work, environment & health, 43(5), 475–484. https://doi.org/10.5271/sjweh.3647
Grippo, A. J., Lamb, D. G., Carter, C. S., & Porges, S. W. (2007). Social isolation disrupts autonomic regulation of the heart and influences negative affective behaviors. Biological psychiatry, 62(10), 1162–1170. https://doi.org/10.1016/j.biopsych.2007.04.011
Afshar, H., Roohafza, H., Sadeghi, M., Saadaty, A., Salehi, M., Motamedi, M., Matinpour, M., Isfahani, H. N., & Asadollahi, G. (2011). Positive and negative perfectionism and their relationship with anxiety and depression in Iranian school students. Journal of research in medical sciences : the official journal of Isfahan University of Medical Sciences, 16(1), 79–86.
Patel, Jainish & Patel, Prittesh. (2019). Consequences of Repression of Emotion: Physical Health, Mental Health and General Well Being. International Journal of Psychotherapy Practice and Research. 1. 16-21. 10.14302/issn.2574-612X.ijpr-18-2564.
Hirotsu, C., Tufik, S., & Andersen, M. L. (2015). Interactions between sleep, stress, and metabolism: From physiological to pathological conditions. Sleep science (Sao Paulo, Brazil), 8(3), 143–152. https://doi.org/10.1016/j.slsci.2015.09.002
Mulkey, S. B., & du Plessis, A. J. (2019). Autonomic nervous system development and its impact on neuropsychiatric outcome. Pediatric research, 85(2), 120–126. https://doi.org/10.1038/s41390-018-0155-0
Pyhälä, R., Wolford, E., Kautiainen, H., Andersson, S., Bartmann, P., Baumann, N., Brubakk, A. M., Evensen, K. A. I., Hovi, P., Kajantie, E., Lahti, M., Van Lieshout, R. J., Saigal, S., Schmidt, L. A., Indredavik, M. S., Wolke, D., & Räikkönen, K. (2017). Self-Reported Mental Health Problems Among Adults Born Preterm: A Meta-analysis. Pediatrics, 139(4), e20162690. https://doi.org/10.1542/peds.2016-2690
Mills, S. E. E., Nicolson, K. P., & Smith, B. H. (2019). Chronic pain: a review of its epidemiology and associated factors in population-based studies. British journal of anaesthesia, 123(2), e273–e283. https://doi.org/10.1016/j.bja.2019.03.023
Schubiner, H., Jackson, B., Molina, K. M., Sturgeon, J. A., Sealy-Jefferson, S., Lumley, M. A., Jolly, J., & Trost, Z. (2023). Racism as a Source of Pain. Journal of general internal medicine, 38(7), 1729–1734. https://doi.org/10.1007/s11606-022-08015-0
Zajacova, A., Grol-Prokopczyk, H., Liu, H., Reczek, R., & Nahin, R. L. (2023). Chronic pain among U.S. sexual minority adults who identify as gay, lesbian, bisexual, or "something else". Pain, 164(9), 1942–1953. https://doi.org/10.1097/j.pain.0000000000002891